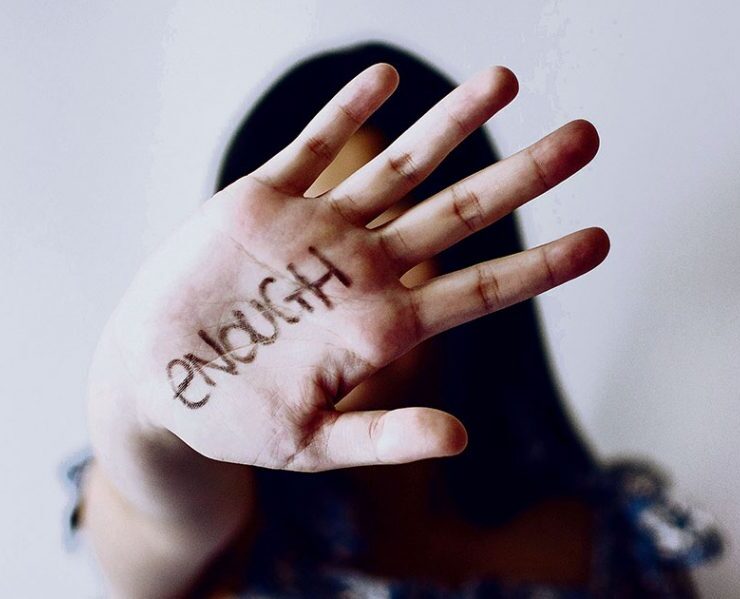
Childhood Depression – Identification and Management

Many people find it almost impossible to associate children’s melancholy, moodiness, and dysphoric mood with depressive disorder. This happens because we typically attribute mood swings in our children to immature and inexperienced actions such as “laziness,” “disorderliness,” and “misbehavior.” Here lies the risk of ignoring a significant and potentially chronic condition such as Generalized Mood Disorder.
There are many who still believe today that such pathology can not exist in children. Unfortunately, though, the percentages and extensive scientific research prove the opposite. The number of depressive children is steadily increasing. The rates rise during the transition to adolescence as they become more detectable, affecting around 20-30%. About one in five children are referred to child psychiatry departments with a diagnosis of depressive disorder.
So, what are the factors that can trigger the onset of the disease?
Genetic and biochemical factors such as certain dysfunctions of specific brain chemicals, and neurotransmitters like serotonin, dopamine, and norepinephrine. Family predisposition, if a first-degree relative suffers from the disease on a stable and long-term basis, constitutes a significant axis of susceptibility. Environmental and social factors such as the loss of a parent, divorce, and family violence (verbal, non-verbal, and physical). Additionally, changing houses, financial problems, and psychological pressures that they induce.

What are the significant clinical symptoms that will lead us to detect the issue?
I use the term “detect” because the parent has the role of a tracker. A very sensitive role plays the balance between imposing boundaries on childish immature behaviours and discovering potential symptoms of a mental illness that might be hidden behind emotional instability, including anger, irritability, laziness, and apathy.
Symptoms
There are three main categories in which the symptoms could be classified.
The first category pertains to emotions and includes irritability, anger, persistent sadness and despair, social withdrawal, heightened sensitivity to any criticism, and feelings of guilt. Additionally, there is a strong sense of worthlessness that undermines the child’s self-esteem.
The second category concerns the Autonomic Nervous System and includes insomnia/hypersomnia, and appetite disturbances (anorexia/overeating, with a link between childhood depression and obesity). Children often associate emotional emptiness or void with consuming high-fat foods to achieve a sense of satiety. Fatigue, exhaustion, loss of energy, and physical discomfort such as headaches and muscle pains are also characteristic of this category.
The third category pertains to the general mental and physical mobilization of the child, and the symptoms are as follows: Significant loss of interest, a feeling of helplessness (believing oneself to be incapable), lack of hope, thoughts of death, and suicidal ideation. It should be emphasized here that a child determined to attempt suicide may give contradictory signals to their environment to avoid arousing suspicion. Therefore, the overall behaviour of the child concerning recent times should be carefully evaluated.
The last category is related to the first and concerns the child’s thinking and perception. The symptoms presented include low self-esteem, thoughts of unworthiness, mnemonic disturbances (difficulty remembering something they were thinking about a second ago), as well as difficulties in concentration. Last, in some cases, and under traumatic shock, it is not unlikely for the child to experience a psychotic episode, losing the flow of speech and thought, and being overtaken by unreal ideas.
Here, I would like to mention that all the above-mentioned symptomatology pertains to children of preschool and school age. However, there is an extremely sensitive category where unfortunately the illness also manifests itself, but it is difficult to detect, and it concerns infants and children of pre-infant age.
Parental Approach
The management of childhood disorders involves therapeutic approaches such as cognitive and behavioral methods that will significantly contribute to problem-solving by teaching the child new ways of thinking and actions that enhance their abilities. Of course, the role of the parent in the approach is crucial.
The parent is the one who must convey to the little one that they are loved and understood, providing an open, supportive embrace for every concern, complaint, and disappointment that may arise. More specifically, it is positive to encourage our children to speak openly about whatever is happening to them without a trace of a critical attitude. The parent must learn the art of being a good listener. This means giving space for the child to express themselves without interruption. Additionally, they should avoid making comments that might make the child feel ashamed and belittle their issue. It would be good to ask specific questions and patiently await the calm and silent response.

We avoid giving advice of the type: “You didn’t do it as I told you” or making diagnoses like “You are sick, that’s for sure” in every possible way. We demonstrate through our behavior (both verbal and non-verbal) that we are there for them, even if we disagree with something they do (always discussing the reasons for our disagreement).
Additionally, we help our child understand that there are different ways to analyze their emotions by providing options for them to realize that even though something seems negative, it may also have positive aspects. We try to develop an action plan involving activities they enjoy (running, cycling, reading fairy tales, playing) and dedicate quality time together. We take their perspective on their self-image very seriously, as this is key to building a strong foundation for their self-esteem. We use learning strategies and techniques that will engage and activate their motivations. We always praise their efforts, both small and large, whenever they succeed in any area.
Lastly, we must not forget that communication, love, patience, accepting their emotions, and recognizing their courage to talk about difficult feelings that overwhelm them are the building blocks of trust between us, as well as the therapeutic journey.
What's Your Reaction?
Family-Systemic Therapist, Speaker, Writer, Blogger